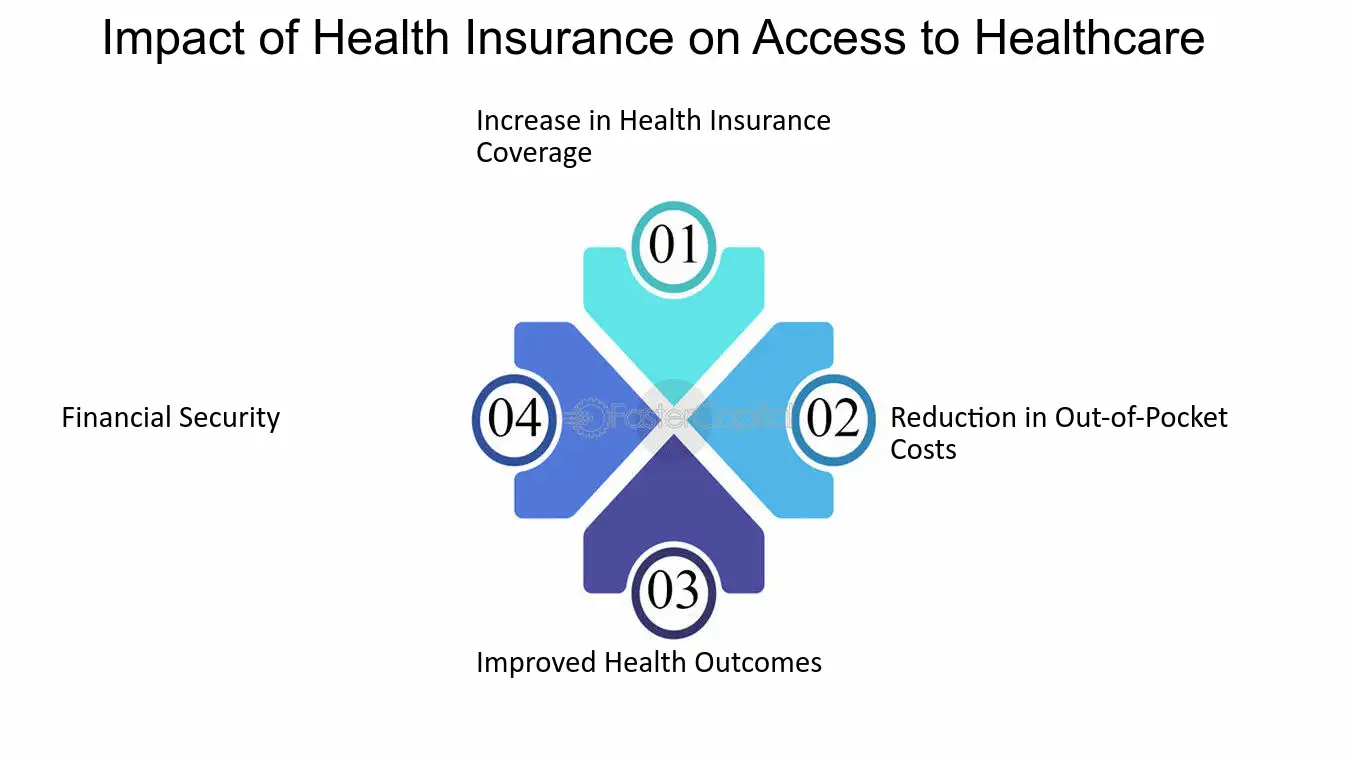
This chapter presents the Committee’s review of studies that address the impact of health insurance on various health-related outcomes. It examines research on the relationship between health insurance (or lack of insurance), use of medical care and health outcomes for specific conditions and types of services, and with overall health status and mortality. There is a consistent, positive relationship between health insurance coverage and health-related outcomes across a body of studies that use a variety of data sources and different analytic approaches. The best evidence suggests that health insurance is associated with more appropriate use of health care services and better health outcomes for adults.
The discussion of the research in this chapter is organized within sections that encompass virtually all of the research literature on health outcomes and insurance status that the Committee identified. The chapter sections include the following:
- Primary prevention and screening services
- Cancer care and outcomes
- Chronic disease management, with specific discussions of diabetes, hypertension, end-stage renal disease (ESRD), HIV disease, and mental illness
- Hospital-based care (emergency services, traumatic injury, cardiovascular disease)
- Overall mortality and general measures of health status
The Committee consolidated study results within categories that reflect both diseases and services because these frameworks helped in summarizing the individual studies and subsumed similar research structures and outcome measures. Older studies and those of lesser relevance or quality are not discussed within this chapter devoted to presenting study results and reaching Committee findings. However, all of the studies reviewed are described briefly in Appendix B.
The studies presented in some detail in this chapter are those that the Committee judged to be both methodologically sound and the most informative regarding health insurance effects on health-related outcomes.1 Most studies report a positive relationship between health insurance coverage and measured outcomes. However, all studies with negative results that are contrary to the Committee’s findings are presented and discussed in this chapter. Appendix B includes summaries of the complete set of studies that the Committee reviewed.
In the pages that follow, the Committee’s findings introduce each of the five major sections listed above and also some of the subsections under chronic disease and hospital-based care. All of the Committee’s specific findings are also presented together in Box 3.12 in the concluding section of this chapter. These findings are the basis for the Committee’s overall conclusions in Chapter 4.
BOX 3.12
Specific Committee Findings. Uninsured adults are less likely than adults with any kind of health coverage to receive preventive and screening services and less likely to receive these services on a timely basis. Health insurance that provides more extensive (more…)
PRIMARY PREVENTION AND SCREENING SERVICES
Finding: Uninsured adults are less likely than adults with any kind of health coverage to receive preventive and screening services and less likely to receive these services on a timely basis. Health insurance that provides more extensive coverage of preventive and screening services is likely to result in greater and more appropriate use of these services.
Finding: Health insurance may reduce racial and ethnic disparities in the receipt of preventive and screening services.
These findings have important implications for health outcomes, as can be seen in the later sections on cancer and chronic diseases. For prevention and screening services, health insurance facilitates both the receipt of services and a continuing care relationship or regular source of care, which also increases the likelihood of receiving appropriate care.
Insurance benefits are less likely to include preventive and screening services (Box 3.2) than they are physician visits for acute care or diagnostic tests for symptomatic conditions. However, over time, coverage of preventive and screening services has been increasing. In 1998, about three-quarters of adults with employment-based health insurance had a benefit package that included adult physical examinations; two years later in 2000, the proportion had risen to 90 percent (KPMG, 1998; Kaiser Family Foundation/HRET, 2000). Yet even if health insurance benefit packages do not cover preventive or screening services, those with health insurance are more likely to receive these recommended services because they are more likely to have a regular source of care, and having a regular source of care is independently associated with receiving recommended services (Bush and Langer, 1998; Gordon et al., 1998; Mandelblatt et al., 1999; Zambrana et al., 1999; Cummings et al., 2000; Hsia et al., 2000; Breen et al., 2001). The effect of having health insurance is more evident for relatively costly services, such as mammograms, than for less costly services, such as a clinical breast exam (CBE) or Pap test (Zambrana et al., 1999; Cummings et al., 2000; O’Malley et al., 2001).
BOX 3.2
Screening Services. The U.S. Preventive Services Task Force (USPSTF) recommends screening for the following conditions in the general adult population under age 65: cervical cancer (above age 18), breast and colorectal cancer (above age 50), hypertension (more…)
According to several large population surveys conducted within the past decade, adults without health insurance are less likely to receive recommended preventive and screening services and are less likely to receive them at the frequencies recommended by the United States Preventive Services Task Force than are insured adults.2 The 1992 National Health Interview Survey (NHIS) documented receipt of mammography, CBE, Pap test, fecal occult blood test (FOBT), sigmoidoscopy, and digital rectal exam by adults under 65 (Potosky et al., 1998). Those with no health insurance had significantly lower screening rates compared to those with private coverage and compared to those with Medicaid for every service except sigmoidoscopy. The odds ratios (ORs) for receiving a screening service if uninsured compared with having private health insurance ranged from 0.27 for mammography to 0.43 for Pap test.3
The 1998 NHIS found that, although rates of screening at appropriate intervals had increased generally over the preceding decade, they remained substantially lower for uninsured adults than for those with any kind of health insurance (Breen et al., 2001).4 In a multivariable analysis that adjusted for age, race, education, and a regular source of care, uninsured adults were significantly less likely than those with any kind of coverage to receive a Pap test, mammography, and colorectal screening (FOBT or sigmoidoscopy) (ORs ranged from 0.37 to 0.5) (Breen et al., 2001). The study reported a strong relationship between having a regular source of care and timely receipt of these screening services in addition to the relationship between health insurance and screening.
Studies using other national samples report results consistent with those of the NHIS. A study of more than 31,000 women between ages 50 and 64 who responded to telephone surveys conducted between 1994 and 1997 about their receipt of mammograms, Pap smears, and colorectal cancer screening (either FOBT or sigmoidoscopy) found that uninsured women were significantly less likely to have received these tests than were women with private prepaid plan insurance (ORs ranging from 0.30 to 0.50) (Hsia et al., 2000). This study also found a strong relationship between having a regular source of care and receipt of screening services. Health insurance was an independently significant predictor. Another study based on several years of the Behavioral Risk Factor Surveillance System (BRFSS) for older adults (55 through 64) found that uninsured men and women were much less likely than their insured counterparts to receive cancer or heart disease screening tests and also much less likely to have a regular source of care (Powell-Griner et al., 1999; see Table 4.1).
Disparities Among Population Groups
A review of the literature on the interaction of race, ethnicity, and socioeconomic status (SES) with health insurance, concluded that health insurance makes a positive contribution to the likelihood of receiving appropriate screening services, although racial and ethnic disparities persist independent of health insurance (Haas and Adler, 2001). Studies of the use of preventive services by particular ethnic groups, such as Hispanics and African Americans, find that health insurance is associated with increased receipt of preventive services and increased likelihood of having a regular source of care, which improves one’s chances of receiving appropriate preventive services (Solis et al., 1990; Mandelblatt et al., 1999; Zambrana et al., 1999; Wagner and Guendelman, 2000; Breen et al., 2001; O’Malley et al., 2001).
Breen and colleagues (2001) modeled the expected increase in screening rates for different ethnic groups if they were to gain health insurance coverage and a regular source of care. This “what-if” model suggests that those groups for whom screening rates are particularly low (e.g., receipt of mammography by Hispanic women, colorectal screening of African-American men) would make the largest gains (an 11 percentage-point increase in mammography rates for Hispanic women [to 77 percent] and a 5 percentage-point increase in colorectal screening for African-American men [to 31 percent] (Breen et al., 2001).
Extensiveness of Insurance Benefits
The type of health insurance and the continuity of coverage have also been found to affect receipt of appropriate preventive and screening services. Faulkner and Schauffler (1997) examined receipt of physical examinations, blood pressure screening, lipid screening for detection of cardiovascular disease, Pap test, CBE, and mammography and identified a positive and statistically significant “dose– response” relationship between the extent of coverage for preventive services (e.g., whether all such services, most, some, or none were covered by health insurance). Insurance coverage for preventive care increased men’s receipt of preventive services more than it did that of women. Men with no coverage for preventive services were much less likely than men with complete coverage for such services to receive them (ORs for receipt of specific services ranged from 0.36 to 0.56). Women with no preventive services coverage also received fewer of these services than did women with full coverage for them (ORs for specific services ranged from 0.5 to 0.83) (Faulkner and Schauffler, 1997).
Ayanian and colleagues (2000) used the 1998 BRFSS data set to analyze the effect of length of time without coverage on receipt of preventive and screening services for adults between ages 18 and 65. Those without coverage for a year or longer were more likely than those uninsured for less than one year to go without appropriate preventive and screening services. For every generally recommended service (mammography, CBE, Pap smear, FOBT, sigmoidoscopy, hypertension screening, and cholesterol screening), the longer-term uninsured were significantly less likely than persons with any form of health insurance to receive these services (Ayanian et al., 2000).
Negative Findings
In the Committee’s review, the one study that did not find a positive effect of insurance coverage compared mammography use among clients of various sites of care in Detroit, Michigan: two health department clinics, a health maintenance organization (HMO), and a private hospital (Burack et al., 1993). This study found no significant differences among women according to their health insurance status but did find that patients with more visits annually for any service (seven or more) were more likely to receive mammography. All women in this study had access to a primary care provider and, in the case of uninsured women, to clinics with the mission of serving the uninsured. These factors may explain why uninsured women had mammography rates as high as those of women with insurance.
CANCER CARE AND OUTCOMES
Finding: Uninsured cancer patients generally have poorer outcomes and are more likely to die prematurely than persons with insurance, largely because of delayed diagnosis. This finding is supported by population-based studies of breast, cervical, colorectal, and prostate cancer and melanoma.
The studies analyzing health-related outcomes for cancer patients provide some of the most compelling evidence for the effect of health insurance status on health outcomes (Box 3.3). This evidence comes from research based on area or statewide cancer registries, which provide large numbers of observations and reflect almost all cases occurring in a geographic region. Multivariable data analysis is used to determine the independent effects of health insurance, by controlling for demographic, SES, and clinical differences among study subjects.
BOX 3.3
Cancer. Cancers of all kinds have an overall incidence nationally of 400 cases per 100,000 people each year. More than 8.9 million Americans alive today have a history of cancer. Cancers account for approximately 550,000 deaths each year in the United (more…)
In addition to receiving fewer cancer screening services, uninsured adults are at greater risk of late-stage, often fatal cancer. Early diagnosis frequently improves the chances of surviving cancer. Generally, in studies examining the stage at which cancer is diagnosed, those with private health insurance have the best outcomes and those with no insurance have the worst (i.e., the highest proportion of late-stage diagnoses), with intermediate outcomes for Medicaid enrollees. In some studies however, the outcomes for Medicaid enrollees are comparable to those for uninsured cancer patients (Roetzheim et al., 1999). Both because of an assumption of similarity in SES between uninsured and Medicaid patients and because of small numbers of observations in the separate categories, some studies report combined results for Medicaid and uninsured patients and compare these findings with those for privately insured patients (e.g., Lee-Feldstein et al., 2000).
In studies assessing the outcomes for adults with cancer—stage of disease at diagnosis and mortality—Medicaid enrollees often do no better, and sometimes do worse, than uninsured patients. This similarity in experience between patients enrolled in Medicaid and those without any coverage may reflect the fact that uninsured persons in poor health, once they seek care, may become enrolled in Medicaid as a result of their frequent interactions with the health care system (Davidoff et al., 2001; see Box 2.1). Also, Medicaid enrollees tend to have discontinuous coverage and thus may have had less regular access to screening services. Consequently, persons with Medicaid at the time of a cancer diagnosis may have been without coverage for some prior period (Carrasquillo et al., 1998; IOM, 2001a; Perkins et al., 2001). For example, one study of women under 65 with Medi-Cal coverage (California’s Medicaid and indigent care program) who were diagnosed with breast cancer found that, among those who had been uninsured during the year prior to their diagnosis (18 percent of all Medi-Cal enrollees), late-stage diagnosis was much more likely than among those who had been continuously enrolled for the previous 12 months (ORs of 3.9 for those who had been uninsured and 1.4 for those continuously covered by Medi-Cal, compared with all other women ages 30–64 diagnosed with breast cancer) (Perkins et al., 2001).
With this general background on the nature of the research examining health insurance status effects, the remainder of this section discusses study results for five specific cancers.
Breast Cancer
Uninsured women and women with Medicaid are more likely to receive a breast cancer diagnosis at a late stage of disease (regional or distant) and have a 30– 50 percent greater risk of dying than women with private coverage, as shown in studies based on three different state or regional cancer registries (Ayanian et al., 1993; Roetzheim et al., 1999, 2000; Lee-Feldstein et al., 2000).
In a study using the New Jersey Cancer Registry, Ayanian and colleagues (1993) identified 4,675 women 35 to 65 years of age diagnosed with breast cancer and assessed their stage of disease at diagnosis and their survival rates 4.5 to 7 years after diagnosis. The authors found that uninsured women were significantly more likely than privately insured women to be diagnosed with regional or late-stage cancer, as were patients with Medicaid. After controlling for stage of disease at diagnosis and other factors, uninsured women had an adjusted risk of death 49 percent higher than that of privately insured women, and women with Medicaid had a 40 percent higher risk of death than those who were privately insured.
Using a regional cancer registry and Census data for 1987 through 1993, Lee-Feldstein and colleagues (2000) examined the stage of disease at diagnosis, treatment, and survival experience of about 1,800 northern California women under the age of 65 diagnosed with breast cancer. They found that women who were uninsured and publicly insured (primarily Medicaid), taken together, were twice as likely as privately insured women with indemnity coverage to be diagnosed at a late stage of disease. Over a four- to ten-year follow-up, uninsured and publicly insured women had higher risks of death from both breast cancer (42 percent higher) and all causes (46 percent higher) than did privately insured women with indemnity coverage. The likelihood of receiving breast-conserving surgery did not differ between these two groups.
In a review of approximately 9,800 Florida residents diagnosed with breast cancer in 1994, Roetzheim and colleagues calculated that, after controlling for age, education, income, marital status, race, and comorbidity, women without insurance were more likely to be diagnosed with late-stage disease than women with private indemnity coverage (OR = 1.43) (Roetzheim et al., 1999). Women with Medicaid had an even greater likelihood of late-stage diagnosis compared with privately insured women (OR = 1.87). In a subsequent analysis of mortality using the same registry data, the authors estimated that the relative risk (RR) of dying was 31 percent higher for uninsured women and 58 percent higher for women with Medicaid over a three to four-year follow-up period (Roetzheim et al, 2000a). Further analysis suggested that stage of disease at diagnosis and, to a lesser extent, treatment modality appeared to account for the differences in survival by insurance status. Finally, uninsured women were less likely than women with private coverage to receive breast-conserving surgery when stage at diagnosis, comorbidities, and other personal characteristics were taken into account (OR = 0.70) (Roetzheim et al., 2000a).
Cervical Cancer
Uninsured women are more likely to receive a late-stage diagnosis for invasive cervical cancer than are privately insured women. Ferrante and colleagues (2000) analyzed 852 cases of invasive cervical cancer reported in the Florida tumor registry for 1994 to determine factors associated with late-stage diagnosis. In bivariate analysis, being uninsured was associated with an increased likelihood of late-stage diagnosis (OR = 1.6). In a multivariable analysis that adjusted for age, education, income, marital status, race, comorbidities, and smoking, uninsured women were more likely to present with a late-stage cancer compared to women with private indemnity coverage, although this finding was not statistically significant (OR = 1.49, confidence interval [CI]: 0.88–2.50). The outcome for Medicaid enrollees was similar to that of privately insured women in both bivariate and multivariable analysis (Ferrante et al., 2000).
Colorectal Cancer
Uninsured patients with colorectal cancer have a greater risk of dying than do patients with private indemnity insurance, even after adjusting for differences in the stage at which the cancer is diagnosed and the treatment modality. Using the Florida cancer registry for 1994, Roetzheim and colleagues (1999) analyzed the relative likelihood of late-stage diagnosis by insurance status for more than 8,000 cases of colorectal cancer. In a multivariable analysis adjusting for sociodemographic characteristics, smoking status, and comorbidities, uninsured patients were more likely to be diagnosed with late-stage colorectal cancer than were patients with private indemnity coverage (OR = 1.67). Medicaid enrollees had a statistically insignificant greater likelihood of late-stage disease compared to patients with indemnity coverage (OR = 1.44, CI: 0.92–2.25).
A subsequent analysis of largely the same data set (9,500 cases) that adjusted for sociodemographic factors and comorbidities but not for smoking estimated the adjusted mortality risk for uninsured patients with colorectal cancer to be 64 percent greater over a three- to four-year follow-up period than that for patients covered by private indemnity plans (Roetzheim et al., 2000b).5 Even after adjusting for stage of disease at diagnosis, the risk of death for uninsured patients was 50 percent higher than that for the privately insured, and after further adjustment for treatment modality, the risk for uninsured patients was 40 percent higher (Roetzheim et al., 2000b).
Prostate Cancer
In addition to delayed diagnosis and greater risk of death, uninsured prostate cancer patients have been found to experience a decrease in health-related quality of life after their diagnosis and during treatment, unlike publicly and privately insured patients. A study of about 8,700 cases of newly diagnosed prostate cancer reported to the Florida cancer registry in 1994 found that uninsured men were more likely to be diagnosed at a late stage of the disease than were men with private indemnity insurance (OR = 1.47) (Roetzheim et al., 1999). A study of 860 men in 26 medical practices with newly diagnosed prostate cancer evaluated their health-related quality of life (HRQOL) at three- to six-month intervals over a two-year period (Penson et al., 2001). Although uninsured men diagnosed with prostate cancer did not have a lower HRQOL at diagnosis, their HRQOL decreased over the course of their disease and treatment, in contrast to that of HMO and Medicare patients. The authors suggest that “patients undergoing aggressive treatment, which can itself have deleterious effects on quality of life, are exposed to further hardships when they do not have comprehensive health insurance upon which to support their care” (Penson et al., 2001, p. 357).
Melanoma
Uninsured patients, as well as Medicaid patients have been found to be more likely to be diagnosed with late-stage melanoma than are privately insured patients. Among 1,500 patients diagnosed with melanoma, uninsured patients were more likely to have late-stage (regional or distant) disease than those with private indemnity coverage (OR = 2.6) (Roetzheim et al., 1999). The small number of Medicaid patients with melanoma (13) included in this study also had a much greater chance of being diagnosed with late-stage cancer.
CHRONIC DISEASE CARE AND OUTCOMES
Finding: Uninsured people with chronic diseases are less likely to receive appropriate care to manage their health conditions than are those who have health insurance. For the five disease conditions that the Committee examined (diabetes, cardiovascular disease, end-stage renal disease, HIV infection, and mental illness), uninsured patients have worse clinical outcomes than insured patients.
Effective management of chronic conditions such as diabetes, hypertension, HIV, and depression (Box 3.4) includes not only periodic services and care from health care professionals but also the active involvement of patients in modifying their behavior, monitoring their condition, and participating in treatment regimens (Wagner et al., 1996; Davis et al., 2000). Identifying chronic conditions early and providing appropriate health care on an ongoing and coordinated basis are health care system goals that have been developed over several decades and have been continuously refined as evidence for cost-effective interventions and practices has accumulated. Maintaining an ongoing relationship with a specific provider who keeps records, manages care, and is available for consultation between visits is a key to high-quality health care, particularly for those with chronic illnesses (O’Connor et al., 1998; IOM, 2001b).
BOX 3.4
Chronic Conditions. Chronic conditions are the leading causes of death, disability, and illness in the United States, accounting for one-third of the potential life years lost before age 65 (CDC, 2000a). Almost 100 million Americans have chronic conditions. (more…)
For persons with a chronic illness, health insurance may be most important in that it enhances the opportunities to acquire a regular source of care. If someone has coverage through a private or public managed care plan, a relationship with a primary care provider may be built into the insurance. Indemnity or fee-for-service (FFS) insurance coverage also improves the chances of having a regular source of care because having the resources to pay for services is often a prerequi-site to being seen in a medical practice. Uninsured adults are much less likely to have a regular source of care and are more likely to identify an emergency department as their regular source of care than are adults with any form of coverage (Weinick et al., 1997; Cunningham and Whitmore, 1998; Zuvekas and Weinick, 1999; Haley and Zuckerman, 2000). Loss of coverage also interrupts patterns of use of health care and results in delays in seeking needed care (Burstin et al., 1998; Kasper et al., 2000; Hoffman et al., 2001). For uninsured adults under age 65, 19 percent with heart disease and 14 percent with hypertension lack a usual source of care, compared to 8 and 4 percent, respectively, of their insured counterparts (Fish-Parcham, 2001). For uninsured patients without a regular source of care or those who identify an emergency department as their usual source, obtaining care that is consistent with recognized standards for effective disease management is a daunting challenge.
Providers with a commitment to serving uninsured clients, such as local public health and hospital clinics and federally funded community health centers, have sometimes instituted special interventions and programs for the chronically ill to promote continuity of care and disease management. These innovations are critically important to the identified, chronically ill patients who routinely receive care at such clinics and centers. The efforts of these providers, however, are limited in scale by funding and service capacity relative to the high need for care within their service areas (Baker et al., 1998; Chin et al., 2000; Piette, 2000; Philis-Tsimikas and Walker, 2001). As demonstrated in the following review of studies examining the care and outcomes for patients with specific chronic conditions, those who do not have health insurance coverage of any kind fare measurably worse than their insured counterparts.
Cardiovascular Disease
Finding: Uninsured adults with hypertension or high cholesterol have diminished access to care, are less likely to be screened, are less likely to take prescription medication if diagnosed, and experience worse health outcomes.
Across the spectrum of services and the course of development of cardiovascular disease (Box 3.5), uninsured adults receive fewer services and experience worse health. They are less likely to receive screening for hypertension and high cholesterol and to have frequent monitoring of blood pressure once they develop hypertension. Uninsured adults are less likely to stay on drug therapy for hypertension both because they lack a regular provider and because they do not have insurance coverage. Loss of insurance coverage has been demonstrated to disrupt therapeutic relationships and worsen control of blood pressure.
BOX 3.5
Cardiovascular Disease. “Cardiovascular disease” encompasses a variety of diseases and conditions that affect the heart and blood vessels, including hypertension (high blood pressure), heart disease, and stroke. One-quarter of all Americans (more…)
Uninsured adults are less likely to receive routine screening services for cardiovascular disease. A nationwide household survey in 1997 found that adults who had been without health insurance for one year or longer were less likely than insured adults to have received recommended hypertension screening within the previous two years (80 percent compared with 94 percent) or cholesterol screening (60 percent compared with 82 percent) (Ayanian et al., 2000). Adults who were uninsured for less than one year received these screening services at rates intermediate between those for long-term uninsured and insured adults.
Health insurance coverage is associated with better blood pressure control for lower-income persons with hypertension, according to two studies, one prospective and experimental and the other a longitudinal analysis of a cohort of patients that either lost or maintained Medicaid coverage. The prospective study, the RAND Health Insurance Experiment, found that for patients with diagnosed hypertension, patients in the plan without any cost sharing had significantly lower blood pressure than those in health plans with any form of cost sharing (an overall difference of 1.9 mm Hg) (Keeler et al., 1985). A much greater effect of cost sharing on average blood pressure was found for low-income patients than for high-income patients (3.5 mm Hg. versus 1.1 mm Hg.). Patients in the plan without cost sharing also had greater compliance with drug and behavioral therapies. These differences were attributed to more frequent contact with health providers in the free care plan (Keeler et al., 1985).6
In the longitudinal analysis, Lurie and colleagues (1984, 1986) followed a cohort of patients at a university ambulatory care clinic for one year after some lost their Medi-Cal coverage consequent to a state policy change. At six months after loss of coverage and again at one year, hypertensive patients who lost coverage had significantly worse blood pressure than did those who remained covered by MediCal, with an average increase in diastolic blood pressure of 6 mm Hg compared with a decrease in the insured control group of 3 mm Hg after a full year (Lurie et al., 1984, 1986). The percentage of patients with diastolic blood pressure greater than 100 mm Hg increased in the group that lost coverage from 3 percent at baseline to 31 percent at six months, and then declined to 19 percent at one year, while the proportion with diastolic blood pressure > 100 mm Hg in the continuously covered control group did not change significantly over the year (Lurie et al., 1986).
Deficits in the care of uninsured persons with hypertension place them at risk of complications and deterioration in their condition. The 1987 National Medical Expenditures Survey afforded an in-depth examination of the use of antihypertensive medications by health insurance status. Uninsured persons younger than 65 who had hypertension were less likely than either those with private insurance or Medicaid to have any antihypertensive medication therapy (ORs = 0.62 and 0.44, respectively) (Huttin et al., 2000).7 An analysis of the third round of the National Health and Nutrition Examination Survey (NHANES), with data on 40,000 respondents for the period 1988–1994, found that 22 percent of uninsured adults under age 65 with diagnosed hypertension had gone for more than one year without a blood pressure check, compared to 10 percent of insured adults with hypertension (Fish-Parcham, 2001). While 75 percent of insured adults under 65 who had ever been diagnosed with high blood pressure and been told to take medication for it were in fact taking blood pressure medication, only 58 percent of their uninsured counterparts who had been advised to take medication were doing so. Among those adults under 65 who had been advised to take cholesterol-lowering medication, 43 percent of those without insurance failed to take such medication, compared to 29 percent among those with health insurance who did not comply with this advice (Fish-Parcham, 2001).
A study by Shea and colleagues (1992a, 1992b) of patients presenting to two New York hospital emergency departments between 1989 and 1991 found that uninsured patients were more likely to have severe, uncontrolled hypertension than were sociodemographically similar patients with any health insurance (OR = 2.2), while patients without a regular source of care had an even greater risk of severe and uncontrolled disease (OR = 4.4). When insurance status, having a regular source of care, and complying with a therapeutic regimen were all included in the analysis, the odds ratio for being uninsured was no longer statistically significant (OR = 1.9, CI: 0.8–4.6). This result is not surprising, given the strong association between having health insurance and having a regular source of care.
Diabetes
Finding: Uninsured persons with diabetes are less likely to receive recommended services. Lacking health insurance for longer periods increases the risk of inadequate care for this condition and can lead to uncontrolled blood sugar levels, which, over time, put diabetics at risk for additional chronic disease and disability.
Despite the demanding and costly care regimen that persons with diabetes face, adults with diabetes are almost as likely to lack health insurance as those without this disease. Of diabetic adults under age 65, 12 percent are uninsured compared with 15 percent of the comparable general population (Harris, 1999). Persons with diabetes who are uninsured are less likely to receive the professionally recommended standard of care than are those who have health insurance (Box 3.6). One result of not receiving appropriate care may be uncontrolled blood sugar levels, which puts diabetics at increased risk of hospitalization for either hyper- or hypoglycemia, in addition to increasing the likelihood of comorbidities and disabilities (Palta et al., 1997).
BOX 3.6
Diabetes. Diabetes mellitus is a prevalent chronic disease that has been increasing in the U.S. population by 5–6 percent each year during the past decade. Approximately 800,000 new cases are diagnosed each year. More than 16 million Americans (more…)
Based on a 1994 survey, among adults diagnosed with diabetes who did not use insulin, those without health insurance were less likely than those with any kind of coverage to self-monitor blood glucose (OR = 0.5) or, within the past year, to have had their feet examined (OR = 0.4), or a dilated eye exam (OR = 0.5) (Beckles et al., 1998).8 Persons with diabetes who used insulin and were uninsured were also less likely than those with health insurance to have had a foot examination (OR = 0.25) or a dilated eye examination (OR = 0.34) (Beckles et al., 1998).
A later analysis, using 1998 data from the same annual survey, found that 25 percent of adults younger than 65 who had diabetes and were uninsured for a year or more had not had a routine checkup within the past two years, compared with 7 percent of diabetics who were uninsured for less than a year and 5 percent of diabetics with health insurance (Ayanian et al., 2000). Adjusting results for the demographic characteristics of the national population, persons with diabetes who were uninsured for a year or longer were significantly less likely to have had a foot examination, a dilated eye examination, a cholesterol measurement, or a flu shot than were insured diabetics (Figure 3.1) (Ayanian et al., 2000).
FIGURE 3.1
Diabetes management among insured and uninsured adults, ages 18–64. NOTE: Proportions adjusted to demographic characteristics of study cohort.
End-Stage Renal Disease
Finding: Uninsured patients with end-stage renal disease begin dialysis at a later stage of disease than do insured patients and have poorer clinical measures of their condition at the time they begin dialysis.
Insurance status affects the timing and quality of care (Box 3.7) and may contribute to the longevity of dialysis patients, which is substantially lower than that of others of the same age (Obrador et al., 1999). The clinical goals for patients with kidney disease are to slow the progression of renal failure, manage complications, and prevent or manage comorbidities effectively. Although professional consensus about when dialysis should begin is not complete, there is agreement that the point in the progression of the disease at which dialysis begins affects patient outcomes (Kausz et al., 2000).
BOX 3.7
End-Stage Renal Disease. In 2000, 90,000 people in the United States developed end-stage renal disease (kidney failure). Dialysis and transplantation are the two standard treatments. Approximately 300,000 patients are on dialysis and 80,000 have received (more…)
The Medicare ESRD program maintains extensive clinical and sociodemographic information on all dialysis patients, including information on patient health insurance status before beginning dialysis. This database provides opportunities to analyze the health care experience of all Americans who eventually develop ESRD, rather than just a sample of the population. One study that used this database analyzed the characteristics of 155,000 chronic dialysis patients who entered dialysis over a 27-month period between 1995 and 1997 (Obrador et al., 1999). This study found that uninsured patients were sicker at initiation of dialysis and less likely to have received erythropoietin (EPO) therapy than patients with any kind of insurance pre-ESRD. Uninsured patients also had an increased likelihood of hypoalbuminemia than those who had previously been privately insured (OR = 1.37) and a greater likelihood of low hematocrit (<28 percent)9 than the privately insured (OR = 1.34), after controlling for patients’ sociodemographic and clinical characteristics, including comorbidities. Uninsured patients were also less likely than privately insured patients to have received EPO prior to dialysis (OR = 0.49) (Obrador et al., 1999). A second study based on the same data set found that patients without insurance were more likely to begin dialysis late10 than were patients with any form of insurance (OR = 1.55) (Kausz et al., 2000).
Human Immunodeficiency Virus (HIV) Infection
Finding: Uninsured adults with HIV infection are less likely to receive highly effective medications that have been shown to improve survival.
A strong body of research about HIV infection confirms the findings of the general literature on insurance status and access to and use of services: uninsured adults diagnosed with HIV face greater delays in care than those with health insurance. They are less likely to receive regular care and drug therapy and are more likely to go without needed care than patients with any kind of coverage (Cunningham et al., 1995, 1999; Katz et al., 1995; Shapiro et al., 1999).
BOX 3.8HIV Infection
- As of the beginning of 2000, the Centers for Disease Control and Prevention estimated that about 800,000 to 900,000 people were living with HIV infection or AIDS in the United States (CDC, 2001a).
- In each of the years 1997, 1998, and 1999, between 40,000 and 50,000 new cases of AIDS were reported.
- By 1996, combination antiretroviral therapy including protease inhibitors and nonnucleoside reverse transcriptase inhibitors, referred to as highly active antiretroviral therapies were becoming established as the treatment of choice for HIV infection (Carpenter et al., 1996). Largely as a result of these therapies, deaths among persons with AIDS dropped for the first time between 1996 and 1997 (by 42 percent) and declined 8 percent between 1998 and 1999 (CDC, 2001a).
- About half of all adults with HIV infection see a provider at least once every six months (Bozzette et al., 1998).
- Studies of HIV infection and health insurance examine a variety of health-related outcomes: general measures of access and utilization such as routine care visits and emergency department visits without hospitalization, delays between diagnosis and initiation of therapy, use of recommended drug therapies, and clinical outcomes such as CD4 lymphocyte counts.
A number of analyses have been based on national, longitudinal surveys evaluating access to care for persons with HIV infection (Niemcryk et al., 1998; Joyce et al., 1999; Shapiro et al., 1999; Andersen et al., 2000; Cunningham et al., 1999, 2000; Turner et al., 2000, Goldman et al., 2001).11 These surveys allow assessment of the relationship between health insurance and access to care, use of services, receipt and timeliness of recommended therapies, and mortality as related to health insurance status. The research based on one of these surveys, the HIV Cost and Services Utilization Study (HCSUS), represents some of the most carefully designed studies of access to care and receipt of recommended therapies for specific conditions. In addition, there are several smaller, local studies based on hospital records or patient surveys (Katz et al., 1992, 1995; Bennett et al., 1995; Cunningham et al., 1995, 1996; Palacio et al, 1999; Sorvillo et al., 1999).
Access to a Regular Source of Care
Several studies suggest that the positive effects of health insurance for HIV-infected adults are achieved through the mechanism of having a regular source of care. Sorvillo and colleagues (1999) surveyed 339 HIV-positive adults in Los Angeles county in 1996–1997, and found that two-thirds of insured patients used protease inhibitors (PIs), while just half of uninsured patients were using them. When the site of care (private clinic, HMO, or public clinic) was included in a multivariable analysis, insurance status was no longer significantly related to receipt of PIs because of the concentration of uninsured patients in public clinics, which were less likely to prescribe PIs, especially at the beginning of the study period (Sorvillo et al., 1999).
Uninsured patients appear to face greater delays in beginning care following a diagnosis of HIV infection. In bivariate analysis of HCSUS data, uninsured patients were significantly more likely to have their first office visit more than three months after diagnosis with HIV than were privately insured patients (37 percent of uninsured patients had delays compared to 25 percent of privately insured patients in 1993; by 1995, those patients with delays decreased to 22 percent of uninsured patients and 14 percent of privately insured) (Turner et al., 2000). However, in a multivariable analysis, being uninsured was no longer a significant predictor of late initiation, while not having a regular source of care remained an important predictor (Turner et al., 2000).
Findings regarding emergency department (ED) use and hospitalization have changed over time. The most recent analysis, based on HCSUS, finds greater use of EDs, without hospitalization, and hospitalization more frequently than every six months for uninsured HIV patients (Shapiro et al., 1999), suggesting poorer access to other kinds of outpatient care. Studies based on earlier data report that uninsured patients had lower use of emergency rooms and hospitalization than either publicly or privately insured patients (Mor et al., 1992; Fleishman and Mor, 1993; Niemcryk et al., 1998; Joyce et al., 1999), suggesting poorer access even at high levels of acuity.
Receipt of Drug Therapies
Adults with HIV infection are more likely to receive effective drug therapies and to receive them earlier in the course of disease if they have health insurance. In an HCSUS analysis with extensive adjustments for sociodemographic and clinical factors, those without health insurance were much less likely to have ever received antiretroviral therapy (OR = 0.35) (Shapiro et al., 1999). Waiting times from diagnosis to the start of therapy with either PIs or nonnucleoside reverse transcriptase inhibitors, were 9.4 months for the privately insured, 12.4 months for Medicaid enrollees, and 13.9 months for uninsured patients (Shapiro et al., 2000).
Overall, many HIV-infected patients abandon recommended drug therapy over time. However, uninsured patients are more likely to stop drug therapy than are those with coverage. At the second follow-up interview of HCSUS respondents in 1997–1998, only half (53 percent) of all HIV-positive patients in care were receiving the recommended combination drug therapy, highly active antiretroviral therapy (HAART), although 71 percent had received HAART at some time in their treatment history (Cunningham et al., 2000). Uninsured patients were significantly less likely than privately insured patients with indemnity coverage (OR = 0.71) to be receiving HAART at the time of follow-up, indicating less appropriate care for uninsured patients with this disease (Cunningham et al., 2000).
Clinical Outcomes and Mortality
Studies of clinical outcomes for HIV patients present an evolving picture of both the efficacy of treatments and the impact of health insurance. A relatively early study of patients hospitalized with Pneumocystis carinii pneumonia (1987– 1990) found that uninsured patients had a higher in-hospital mortality rate than did those with private insurance (OR = 1.49), and Medicaid patients had an even higher in-hospital mortality, relative to private patients (OR = 2.1) (Bennett et al., 1995). Another early and small study (96 patients in one university clinic) found that patients with private insurance had significantly lower CD4 lymphocyte counts (a worse outcome) than either uninsured or Medicaid patients (who had the highest counts), when first treated at the clinic (Katz et al., 1992). The authors hypothesize that some relatively healthy patients with private health insurance coverage may have been reluctant to use it and thus reported their status as uninsured.
More recently, an analysis based on HCSUS examined the mortality experience of insured and uninsured HIV-infected adults and found that having health insurance of any kind reduced the risk of dying within six months of being surveyed between 71 and 85 percent, when severity of illness (measured by CD4 lymphocyte count) and sociodemographic characteristics were controlled (Goldman et al., 2001). The greater reduction in mortality risk (85 percent) was estimated for a surviving subset (2,466 participants) of the original 1996 sample of 2,864 participants a year later, when HAART was in wider use and was reducing mortality among HIV patients who used it. This impact of health insurance on mortality for HIV-infected adults within a short follow-up period, six months, demonstrates how sensitive health outcomes can be to coverage when it facilitates receipt of effective therapy.
Mental Illness
Finding: Health insurance that covers any mental health treatment is associated with the receipt of mental health care and with care consistent with clinical practice guidelines from both general medical and specialty mental health providers.
Mental disorders or illnesses are health conditions that are characterized by changes in thinking, mood, or behavior. They are often chronic conditions but may also occur as single or infrequent episodes over a lifetime. Mental illnesses represent a major source of disability in the United States that is often underestimated by the public and health care professionals alike (USDHHS, 2000). In industrialized economies, mental illness is equivalent to heart disease and cancer in terms of its impact on disability (Murray and Lopez, 1996).
Despite the differential treatment of mental health services in both public and private insurance plans, the studies reviewed by the Committee document a positive association between health insurance coverage and more appropriate care for mental illnesses (Box 3.9). Health insurance plans and programs historically have excluded services related to treatment for mental illness, strictly limited coverage of mental health services, and administered mental health benefits separately from other kinds of medical care. Thus, studies that attempt to measure the effects of health insurance status on health care and outcomes for mental illnesses may be affected by the diversity of health insurance benefits and of cost sharing and administrative requirements for these services and conditions. Variability in benefits among health insurance plans and types of insurance complicates the interpretation of all observational studies of health insurance effects but poses a particular problem vis–a–vis mental health. (See the discussion of measurement bias in Chapter 2.)
BOX 3.9
Mental Illness. About 38 million people ages 18 and older are estimated to have a single mental disorder of any severity or both a mental and an addictive disorder in a given year (Narrow et al., 2002). The most common conditions fall into the broad categories (more…)
The use of mental health services in both the general and specialty mental health sectors by adults is positively associated with health insurance coverage (Cooper-Patrick et al., 1999; Wang et al., 2000; Young et al., 2001). Between 1987 and 1997, the overall rate of treatment for depression among American adults under age 65 tripled from 1 person per 100 to 3.2 persons per 100, yet the treatment rate among those without health insurance was half that of the overall population rate in 1997, 1.5 persons treated per 100 population (Olfson et al., 2002). A longitudinal, community-based study in Baltimore, Maryland, between 1981 and 1996 documented increased use of mental health services over this period (Cooper-Patrick et al., 1999). Analyzing the experience of African Americans and whites separately, the authors found that for African Americans specifically, this increase was achieved predominantly with services provided in the general medical sector. For both African Americans and whites, being uninsured reduced the likelihood of receiving any mental health services.
At the same time, insurance coverage for adults with mental illness is less stable than average for those without this condition (Sturm and Wells, 2000; Rabinowitz et al., 2001). In a recent (1998) follow-up survey of participants in the Community Tracking Study, those who reported having symptoms of mental disorders were found to be more likely to lose coverage within a year following their diagnosis than those without a mental disorder (Sturm and Wells, 2000). As discussed below, those with severe mental illness also experience transitions in insurance coverage, frequently ending up with public program coverage (Rabinowitz et al., 2001).
The findings reported below are grouped into those for depression and anxiety disorders and those for severe mental illnesses. Depression and anxiety disorders are often treatable in the general medical sector and primarily require outpatient services. Severe mental illnesses (schizophrenia, other psychoses, and bipolar depression) require the attention of specialty mental health professionals and may require inpatient and other forms of more extensive services (e.g., partial or day hospitalization). Public health insurance, both Medicare and Medicaid, is an important source of coverage for specialty mental health services for those disabled by severe mental illness (SMI).
Depression and Anxiety Disorders
Receipt of appropriate (guideline-concordant) care for depression is associated with improved functional outcomes at two years (Sturm and Wells, 1995). Health insurance coverage specifically for mental health services is associated with an increased likelihood of receiving such care. Two studies support this claim.
The first, a nationally representative study of three prevalent disorders— depression, panic disorder, and generalized anxiety disorder—investigated the contribution of insurance coverage and health care utilization to guideline-con-cordant treatment (Wang et al., 2000). Mental health diagnoses were determined in a structured interview using a well-defined operational definition of mental health care over the previous 12 months. Treatment criteria included the combination of a prescription medication for depression or anxiety from a general medical doctor or a psychiatrist in addition to at least four visits to the same type of provider or, where medication was not prescribed, a minimum of eight visits to either a psychiatrist or a mental health specialist (Wang et al., 2000). A multivariable analysis estimated the effects of sociodemographic characteristics, various measures of clinical status including a measure of mental illness severity, insurance coverage for mental health visits, number and reasons for use of general medical services, other medications, and alternative therapies. Patients diagnosed with depression, panic disorder, or a generalized anxiety disorder who had no health insurance coverage for mental health visits were less likely to receive any mental health services (OR = 0.43). They were also less likely to receive guideline-concordant care in the general medical sector (OR = 0.24) or in the mental health treatment sector (OR = 0.36) (Wang et al., 2000).
A second study of adults with a probable 12-month diagnosis of depression or anxiety examined factors associated with receipt of appropriate care (psychiatric medication and counseling) (Young et al, 2001): 1,636 respondents were identified as having one or more depressive or anxiety disorders based on a structured diagnostic interview. Respondents with a depressive or anxiety disorder who had more education and a greater number of medical disorders were more likely to have had contact with providers than those with less education and fewer medical conditions. Those with no health insurance were less likely to have had any provider contact than were those with any form of health insurance (OR = 0.46). However, for those receiving any care, insurance status was not related to receipt of appropriate care (Young et al., 2001). These findings suggest that health insurance alone may not ensure appropriate mental health care.
Severe Mental Illness
Uninsured adults with severe mental illnesses are less likely to receive appropriate care than are those with coverage and may experience delays in receiving services until they gain public insurance.
In a study using the same sample and survey as that used by Young and colleagues, McAlpine and Mechanic (2001) investigated the association of current insurance coverage and specialty mental health utilization within the past 12 months (i.e., visits to a psychiatrist or psychologist, hospital admission, or emergency room visit for an emotional or substance use problem) for SMI. Two diagnostic indices, including a global measure of mental health, measured the need for care. Potential confounding factors such as physical symptoms and degree of dangerousness and disruptiveness were also measured. One in five respondents identified with an SMI was uninsured. Among persons with SMI, those without health insurance were far less likely to use specialty mental health services than those with Medicare or Medicaid (OR = 0.17) (McAlpine and Mechanic, 2000).
Individuals with SMIs typically lack insurance at the time of hospitalization (Rabinowitz et al., 2001). An important question regarding insurance coverage in this patient population is whether a first hospitalization for SMI results in a change in insurance status and whether such a change influences subsequent mental health care. Rabinowitz and colleagues followed the progress of 443 individuals enrolled in a county mental health project to determine whether changes in coverage followed first admission for psychosis and the association between type of insurance coverage and future care. Overall, the proportion of patients with no insurance 24 months after hospitalization decreased from 42 percent at baseline to 21 percent as a result of enrollment in public insurance programs. Men were more likely to remain uninsured than were women. The total number of days of care received (inpatient, outpatient, day hospital) was significantly higher for the publicly insured group compared to both those with private insurance and those with no insurance during the first 6 months after initial hospitalization and over the entire 24-month period. Uninsured patients with SMI were much less likely to receive outpatient care after hospitalization than patients with Medicaid or Medicare (OR = 0.24) and also less likely than those with private health insurance to receive outpatient care subsequent to hospitalization (OR = 0.56) (Rabinowitz et al., 2001).
An earlier study using the same data also reported an association between health insurance and receipt of mental health services prior to a first admission for psychotic disorder (Rabinowitz et al., 1998). Forty-four percent of patients (n = 525) were uninsured at first admission. Uninsured patients were less likely than those with private insurance to have had
- any mental health treatment prior to admission (OR = 0.53),
- specific psychotherapeutic contact (OR = 0.43),
- voluntary admission (OR = 0.56),
- less than three months between onset of psychosis and admission (OR = 0.56)
and were less likely to have been admitted to a community (versus public) hospital (OR = 0.14) (Rabinowitz et al., 1998). Uninsured patients were also less likely than those with either Medicaid or Medicare to have received antipsychotic medication (OR = 0.4), had voluntary admission (OR = 0.53), and be admitted to a community hospital (OR = 0.33).
HOSPITAL-BASED CARE
Finding: Uninsured patients who are hospitalized for a range of conditions experience higher rates of death in the hospital, receive fewer services, and are more likely to experience an adverse medical event due to negligence than are insured patients.
Americans assume and expect that hospital-based care for serious and emergency conditions is available to everyone, regardless of health insurance coverage, while recognizing that uninsured patients may be limited to treatment at public or otherwise designated “safety-net” hospitals (IOM, 2001a). Professional and institutional standards of practice grounded in ethics, law, and licensure dictate that the care received by all patients, regardless of financial or insurance status, be of equal and high quality. Yet studies of hospital-based care conducted over the past two decades have documented differences in the services received by insured and uninsured patients, differences in the quality of their care (sometimes but not always related to the site of care), and differences in patient outcomes such as in-hospital mortality rates.12
One of the most comprehensive of these studies of hospitalization analyzed more than 592,000 hospital discharge abstracts in 1987 (Hadley et al., 1991). The authors report that for adults ages 18–65, uninsured hospital inpatients had a significantly higher risk of dying in the hospital than their privately insured counterparts in 8 of 12 age–sex–race-specific population cohorts (relative risks ranged from 1.1 for black women ages 50–64 to 3.2 for black men ages 35–49). This analysis adjusted for patient condition on admission to the hospital. Uninsured patients were also less likely to receive endoscopic procedures in the hospital than privately insured patients, and when they did receive these diagnostic services, the resultant pathology reports were more likely to be abnormal (OR = 1.56) (Hadley et al., 1991).
This study by Hadley and colleagues also examined the relative resource use (length of stay) of uninsured hospital patients compared to privately insured patients and found that for conditions that afford high discretion in treatment decisions (e.g., tonsillitis, bronchitis, hernia), uninsured patients had significantly shorter lengths of stay (Hadley et al., 1991). However, for diagnoses that afford little discretion in treatment (e.g., gastrointestinal hemorrhage, congestive heart failure), lengths of stay were not significantly different for uninsured and privately insured patients, although uninsured patients tended to have shorter stays. This underscores the possibility that when uninsured patients are found to receive fewer services than insured patients, it may be the result of overtreatment of patients with insurance, rather than undertreatment of those without coverage.
In addition to differences in the resources devoted to the care of insured and uninsured patients, the quality of the care provided may differ. One study of more than 30,000 hospital medical records in 51 hospitals in New York State for 1984 found that the proportion of adverse medical events due to negligence was substantially greater among patients without health insurance than among privately insured patients (OR = 2.35), while the experience of Medicaid patients did not differ significantly from that of the privately insured population (Burstin et al., 1992). This increased risk for uninsured patients was attributable only in part to receiving care more frequently in emergency departments, which generally were found to have higher rates of adverse events.
Because most studies of hospital-based care and outcomes are observational, including only those who literally “show up” for care, and because appropriateness criteria are not available for many conditions, some of the strongest research on health insurance effects involves studies of specific conditions. Studies of certain conditions are less likely to be compromised by nonrandom or unrepresentative samples (selection bias) simply because a larger proportion of the population of interest—namely, acutely ill adults—is likely to be captured in the hospital-based study population. Furthermore, condition-specific studies are more likely to include evidence-based criteria for judging the appropriateness of care.
The following two sections consider research that has examined the effect of health insurance on care and outcomes for patients with (1) emergency conditions and traumatic injuries and (2) cardiovascular disease. For both categories, selection bias among those reaching treatment is minimized, and appropriateness guidelines and outcomes criteria (e.g., mortality) are definitive. Traumatic injuries (specifically automobile accidents), for example, reduce some of the unmeasured differences in propensity to seek care between insured and uninsured patients (Doyle, 2001). Another area of hospital-based services for which there is sufficient professional consensus about appropriate treatment is the use of angiography and revascularization procedures following acute myocardial infarction (AMI) or heart attack, at least for a subset of patients with severe coronary artery disease.13
Emergency and Trauma Care
Finding: Uninsured persons with traumatic injuries are less likely to be admitted to the hospital, receive fewer services when admitted, and are more likely to die than insured trauma victims.
Two studies based on large, statewide data sets have found substantial and significant differences in the risk of dying for insured and uninsured trauma patients (Box 3.10) who were admitted to hospitals as emergencies. Doyle (2001) analyzed more than 10,000 police reports of auto accidents linked to hospital records maintained by Wisconsin over 1992–1997 to ascertain the care received and the mortality of insured and uninsured crash victims. After controlling for personal, crash, and hospital characteristics, it was found that uninsured accident victims received 20 percent less care, as measured by hospital charges and length of stay, and had a 37 percent higher mortality rate than did privately insured accident victims (5.2 percent versus 3.8 percent, respectively) (Doyle, 2001). The authors conclude that these differences are attributable to provider response to insurance status because extensive patient characteristics were accounted for in the analysis and because unmeasured patient characteristics that might influence these outcomes were unlikely to be related to patients’ health insurance status.
BOX 3.10
Trauma. Throughout the United States in 1997, approximately 34.4 million episodes of injury and poisoning received medical attention and 40.9 million injuries and poisonings were reported as a result (Warner et al., 2000). For injury-related deaths, 43 (more…)
Haas and Goldman (1994) evaluated the treatment experience and mortality of more than 15,000 insured and uninsured trauma patients admitted to hospitals on an emergency basis in Massachusetts in 1990. Adjusting the data for injury severity and comorbidities as well as for age, sex, and race, the authors found that uninsured trauma patients received less care and had higher in-hospital mortality than did patients with private insurance or Medicaid. Uninsured patients were just as likely to receive care in an intensive care unit (ICU) as privately insured trauma patients but were less likely to undergo an operative procedure (OR = 0.68) or to receive physical therapy (OR = 0.61). Uninsured patients were much more likely than privately insured patients to die in the hospital (OR = 2.15) (Haas and Goldman, 1994). The differences in services and mortality experience between Medicaid and privately insured patients were small and were not statistically significant.
Other studies of emergency department use and admissions and care for traumatic injuries shed some light on patient behavior and institutional responses related to health insurance status. Both lacking health insurance and not having a regular source of care have been found in surveys of patients who eventually do arrive at an ED to be related to delays in seeking care (Ell et al., 1994; Rucker et al., 2001). Braveman and colleagues (1994) examined hospital discharge records of more than 91,000 adults diagnosed with acute appendicitis in California hospitals between 1984 and 1989. They found that the risk of a ruptured appendix was 50 percent higher for both uninsured and Medicaid patients, than for privately insured patients in prepaid plans, in an analysis that controlled for age, sex, race, psychiatric diagnoses, diabetes, and hospital characteristics. Admission to a public hospital also was associated with rupture, as were diagnoses of psychiatric illness or diabetes (Braveman et al., 1994). The authors hypothesized that both Medicaid and uninsured patients incurred avoidable delays before seeking care for appendicitis.
Three separate studies that analyzed Medicaid and uninsured trauma patients together report mixed findings regarding patient outcomes and hospital care. Rhee and colleagues (1997) examined patient information for more than 2,800 persons hospitalized at a Level 1 trauma center after a motor vehicle crash in Seattle, Washington, between 1990 and 1993.14 This study found no significant differences in mortality, hospital charges, or length of stay (LOS) between privately insured patients and those who either had Medicaid coverage or were uninsured, except for patients who ultimately were transferred to a long-term care or rehabilitation facility. In the case of patients awaiting transfer, those with Medicaid or no insurance had an adjusted LOS that was 11 percent longer than privately insured patients (Rhee et al., 1997). The authors speculate that the similarity in treatment and outcomes for patients of different insurance status could be due to the mission of the public, Level 1 trauma center to which they were admitted, which was to serve the entire state population needing that level of care and act as a provider of last resort for uninsured patients. Because this study did not differentiate results for Medicaid and uninsured patients, it provides less information about outcomes for uninsured patients than studies that analyze these groups separately.
Uninsured trauma patients may also be treated differently from insured patients in interhospital transfer decisions. Using Washington State trauma registry information, Nathens and colleagues (2001) identified 2,008 trauma patients between 16 and 64 years of age injured in King County (Seattle) and originally transported to one of seven Level 3 or 4 trauma centers in the county between 1995 and 1999. Adjusting for age, sex, type of injury, and injury severity, they looked at independent predictors of transfer to the Level 1 trauma center in the county—a public, safety-net hospital, and estimated that patients who either had Medicaid or were uninsured were more than twice as likely to be transferred to the higher level facility than were privately insured patients (OR = 2.4) and that many of these transferred patients had low injury severity scores (ISS).15 The authors conclude that this “payer-based triage” may undermine the effectiveness of Level 1 trauma centers in serving the more critically injured patients by diverting resources to patients who could have been treated appropriately in their original hospital (Nathens et al., 2001).
Finally, the differences found between uninsured and insured patients in highly discretionary cases may reflect overtreatment of those with health insurance rather than undertreatment of uninsured patients. Svenson and Spurlock (2001) evaluated the experience of more than 8,500 patients with head injuries treated in four Kentucky hospitals between 1995 and 1997. For those with less severe head injuries (lacerations, contusion, or concussion), uninsured patients were substantially less likely than privately insured patients to be admitted to the hospital (OR = 0.14 for laceration, 0.38 for contusion or concussion). The likelihood of admission for Medicaid was also substantially lower than for privately insured patients, but not as low as for uninsured patients (ORs = 0.33 and 0.45, respectively). Little difference was found in hospital admissions for more severe head injuries among patients with different insurance status. The authors were unable to determine whether the differences in admissions for less severe head trauma are due to undertreatment of uninsured and Medicaid patients or overtreatment of privately insured patients (Svenson and Spurlock, 2001).
Cardiovascular Disease
Finding: Uninsured patients with acute cardiovascular disease are less likely to be admitted to a hospital that performs angiography or revascularization procedures, are less likely to receive these diagnostic and treatment procedures, and are more likely to die in the short term.
Finding: Health insurance reduces the disparity in receipt of these services by members of racial and ethnic minority groups.
Health insurance is positively associated with receipt of hospital-based treatments for cardiovascular disease (specifically, coronary artery disease) and with lower patient mortality (Box 3.11). One meta-analysis has credited medical advances in the treatment of cardiovascular disease, including hospital-based care following AMI, with roughly half of the reduction in post-AMI mortality between 1975 and 1995 (with a range of 20 to 85 percent) (Cutler et al., 1998). Some of the most recent studies have used appropriateness criteria to identify when a given procedure is considered necessary according to professional consensus, reducing the chances that differences in rates between uninsured and insured patients are a result of overtreatment of the insured population (i.e., Sada et al.,1998; Leape et al., 1999).
BOX 3.11
In 2001, an estimated 1.1 million Americans suffered a diagnosed heart attack. An estimated 7.3 million Americans have a history of AMI (American Heart Association, 2001). During 1998, coronary heart disease accounted for about 460,000 deaths; AMI was (more…)
Mortality
Five studies that examined the mortality experience of patients hospitalized for cardiovascular disease (including AMI, angina, and chest pain) reported higher in-hospital or 30-day posthospitalization mortality for uninsured patients (Young and Cohen, 1991; Blustein et al., 1995; Kreindel et al., 1997; Sada et al., 1998; Canto et al., 2000).
The first study, of about 5,000 patients admitted on an emergency basis for AMI in 1987, found that uninsured patients were more likely to die within 30 days of admission than privately insured patients (OR = 1.5) (Young and Cohen, 1991). In a second study, Blustein and colleagues (1995) examined records for 5,800 patients under 65 who were admitted to California hospitals for AMI in 1991 and found that uninsured patients were more likely to die in the hospital than privately insured patients (OR = 1.9) and still had an increased risk of dying after adjusting for receipt of a revascularization procedure (OR = 1.7). Finally, a study in a single Massachusetts community of 3,700 patients hospitalized for AMI between 1986 and 1993 reported that uninsured patients had a slight, but statistically insignificant greater in-hospital mortality than privately insured patients (OR = 1.2, CI: 0.6–2.4) (Kreindel et al., 1997).
Two larger studies that used more recent data (1994–1996) from the National Registry of Myocardial Infarction reported higher in-hospital mortality for uninsured than for privately insured patients. In the first, Sada and colleagues (1998) reviewed records for 17,600 patients under age 65 who were admitted to hospital for AMI and found that uninsured patients had an in-hospital mortality rate of 5.4 percent, compared with 3.8 percent for private FFS patients and 3.9 percent for private HMO patients. Medicaid patients had the highest in-hospital mortality rate, 8.9 percent. In a model that adjusted for demographic and clinical factors, the likelihood of uninsured patients dying in the hospital was still higher but was not statistically significantly different from that of privately insured patients (OR = 1.2, CI: 0.8–1.6) (Sada et al, 1998). The second national study examined records for more than 332,000 patients admitted with AMI and found that after adjusting for demographics, prior disease history, and clinical characteristics, uninsured patients were more likely to die in the hospital than privately insured FFS patients (OR = 1.29) (Canto et al., 2000). The mortality experience of Medicaid patients was the same as that of uninsured patients.
Only one study, a review of hospital records of 1,556 patients undergoing coronary artery bypass graft surgery in a single Louisiana teaching hospital, found that uninsured patients had better long-term survival than did insured patients (Mancini et al., 2001). However, this study did not control for age or characteristics of the patients. The average age of uninsured patients at the time of surgery was 55, and of insured patients, 65 years. Furthermore, only 7 percent of the insured study population had private insurance, so the population was not representative of the insured population at large.
Coronary Procedures
The body of research on the use of specific procedures to diagnose and treat cardiovascular disease as a function of the insurance status of the patient consistently reports differences in utilization, with uninsured patients generally less likely to receive coronary angiography, CABG, or percutaneous transluminal coronary angioplasty (PTCA) than privately insured patients (Young and Cohen, 1991; Blustein et al., 1995; Kuykendall et al., 1995; Sada et al., 1998; Leape et al., 1999; Canto et al., 2000; Daumit et al., 2000). However, only some of these studies applied appropriateness criteria to identify cases in which the use of these procedures was considered nondiscretionary or necessary. In the studies that examined overall utilization rates, the differences found by insurance status could be attributed to overutilization as well as underutilization.
Angiography (cardiac catheterization) is an invasive diagnostic procedure that provides information to guide decisions about subsequent treatment options, including revascularization procedures. Sada and colleagues (1998) applied the criteria of the American College of Cardiology and American Heart Association Joint Task Force to a national data set of 17,600 myocardial infarction patients under 65 to identify nondiscretionary angiography for revascularization candidates considered to be at high risk. They estimated that in hospitals providing these cardiac procedures, patients with private FFS coverage who were deemed high-risk and for whom angiography was nondiscretionary were more likely than similarly high-risk uninsured patients or Medicaid patients to receive angiography. Among high-risk FFS patients, 84 percent received this service compared to 73 percent of high-risk uninsured patients and 60 percent of similar Medicaid patients (Sada et al., 1998).
Revascularization procedures (either CABG or PTCA) following a heart attack are also more likely to be performed on insured than uninsured patients. In two studies, uninsured patients were less likely to receive revascularization (either CABG or PTCA) than privately insured FFS patients (OR = 0.6 in the 1991 study and 0.8 in the 2000 study) (Young and Cohen, 1991; Canto et al., 2000). Blustein and colleagues (1995) and Kuykendall and colleagues (1995) reported similar comparative findings regarding the revascularization of uninsured and privately insured patients (ORs in these studies ranged from 0.4 to 0.6).
InterHospital Transfers to Receive Services. For patients with AMI, health insurance facilitates access to hospitals that perform angiography and revascularization, whether admission is initial or by means of an interhospital transfer (Blustein et al., 1995; Canto et al., 1999; Leape et al., 1999).
In a study of California hospital admissions for AMI, Blustein and colleagues (1995) found that uninsured patients were less likely than privately insured patients to be admitted initially to a hospital that offered revascularization and much less likely to be transferred if admitted initially to one that did not (ORs = 0.71 and 0.42, respectively).
Leape and colleagues (1999) reviewed 631 records for patients who had received angiography and subsequently met expert panel criteria for necessary revascularization. Overall, 74 percent of patients meeting these criteria received revascularization. Leape et al. found that in hospitals that also performed CABG and PTCA, there were no differences in rates of revascularization for patients with different insurance status. However, for patients initially hospitalized in facilities that did not perform CABG and PTCA, who required a transfer to another hospital to receive revascularization, the rates differed significantly by insurance status: 91 percent of Medicare patients, 82 percent of privately insured patients, 75 percent of Medicaid patients, and just 52 percent of uninsured patients received this indicated surgery (Leape et al., 1999).
Insurance Status and Racial and Gender Disparities. Health insurance has been shown to lessen disparities in the care for cardiovascular disease received by men compared to women and among members of racial and ethnic groups (Carlisle et al., 1997; Daumit et al., 1999, 2000).
An analysis of more than 100,000 hospital discharges with a principal diagnosis of cardiovascular disease in Los Angeles County between 1986 and 1988 revealed significant differences in rates of angiography, CABG, and PTCA between uninsured African-American and white patients but not between members of these ethnic groups who were privately insured (Carlisle et al., 1997). In a multivariate analysis that controlled for demographic and clinical characteristics and hospital procedure volume, the odds ratios for uninsured African Americans to receive one of these services compared with uninsured whites ranged from 0.33 to 0.5 (Carlisle et al., 1997).
A longitudinal study with a seven-year follow-up of a national random sample of patients who initially became eligible for the Medicare ESRD program in 1986 or 1987 found that once uninsured patients qualified for ESRD benefits, pronounced disparities by gender or race in their likelihood of receiving either angiography, CABG, or PTCA were eliminated (Daumit et al., 1999, 2000). In the period prior to qualifying for Medicare, uninsured African Americans were far less likely than uninsured whites to undergo a cardiac procedure (OR = 0.07) (Daumit et al., 1999). Uninsured women were also less likely than uninsured men to receive a cardiac procedure before qualifying for Medicare (OR = 0.4), and uninsured men were much less likely than men with private insurance to receive one (OR = 0.47) (Daumit et al., 2000). In the case of both race and gender, differences in the receipt of these cardiac procedures were eliminated after gaining Medicare ESRD coverage.
GENERAL HEALTH OUTCOMES
Finding: Longitudinal population-based studies of the mortality of uninsured and privately insured adults reveal a higher risk of dying for those who were uninsured at baseline than for those who initially had private coverage.
Finding: Relatively short (one- to four-year) longitudinal studies document relatively greater decreases in general health status measures for uninsured adults and for those who lost insurance coverage during the period studied than for those with continuous coverage.
This chapter concludes with a review of the studies evaluating the overall health status and mortality experience of insured and uninsured populations. Assessments of general health outcomes such as self-reported health status and mortality or survival rates for uninsured adults under 65 compared to those with some form of health insurance (i.e., employment-sponsored, Medicaid, Medicare, individually purchased policies), present researchers with even greater challenges of analytic adjustment than those encountered in studies of specific health conditions. Not only might health insurance affect health status, but health status can affect health insurance status. Thus, it is difficult to interpret cross-sectional studies of health insurance and health status. However, several well-designed longitudinal studies with extensive analytic adjustments for covariates have found higher mortality and worse overall functional and health status among uninsured adults than among otherwise similar insured adults.
Mortality
Two studies provide evidence that uninsured adults are more likely to die prematurely than are their privately insured counterparts.
Franks and colleagues (1993a) followed a national cohort of 4,700 adults age 25 or older for 13 to 17 years who, at the baseline interview, were either privately insured or uninsured. At the end of the follow-up period (1987), about twice as many participants who were uninsured at the time of the first interview had died as had those with private health insurance (18.4 percent compared with 9.6 percent). Controlling for sociodemographic characteristics, health examination findings, self-reported health status, and health behaviors, the risk of death for adults who initially were uninsured was 25 percent greater than for those who had private health insurance at the time of the initial interview (mortality hazard ratio = 1.25, CI: 1.00–1.55). The magnitude of this independent health insurance effect on mortality risk was comparable to that of being unemployed, to lacking a high school diploma, or to being in the lowest income category (Franks et al., 1993a).16 Because insurance status was measured only at the initial interview and thus did not reflect the subjects’ cumulative insurance experience over the 13–17 year follow-up period, the difference found in mortality between uninsured and privately insured persons most likely is an underestimate of differences in the mortality experience of those who are continuously uninsured and those who are continuously insured.
A study by Sorlie and colleagues (1994) tracked the mortality experience of 148,000 adults between 25 and 65 years of age until 1987, a two- to five-year follow-up period. After adjusting for age and income, this study found that uninsured white men had a 20 percent higher risk of dying than white men with employment-based health insurance. Uninsured black men and white women each had a 50 percent higher mortality risk than their counterparts with employment-based coverage (Sorlie et al., 1994). Among black women, insurance was not statistically associated with mortality. The authors also examined the mortality experience of insured and uninsured employed white men and women, adjusted for age and income. (Because of small sample size, they did not perform this analysis for black men and women.) Uninsured employed white men had a 30 percent greater risk of dying than their working counterparts with health insurance, and uninsured employed white women had a 20 percent greater risk over two to five years than their counterparts with health insurance (Sorlie et al., 1994).
Loss of Coverage and Changes in Health Status Over Time
Persons who lose health insurance have been found to experience declines in their health status. Longitudinal studies that follow a cohort of individuals over time can provide a “before-and-after” picture of health status, comparing a group that maintained coverage with one that lost it. Such a design helps to minimize the possibility that unmeasured factors that vary along with health insurance status account for differences in health, a competing hypothesis that cannot be eliminated in cross-sectional studies.
Lurie and colleagues (1984, 1986) took advantage of a natural experiment in the mid-1980s when California eliminated Medi-Cal coverage for a group of medically indigent adults. Following matched cohorts of adults seen at an internal medicine practice at a university clinic who either maintained or lost Medi-Cal coverage, the authors found that the patients who lost coverage reported significant decreases in perceived overall health at both six months and a year later, unlike those who maintained coverage. As discussed earlier in this chapter, participants in this study with hypertension who lost coverage also experienced worsening blood pressure control, while those who maintained coverage did not.
Like those with chronic health conditions, adults in late middle age are particularly susceptible to deteriorations of function and health status if they lack or lose health insurance coverage. Baker and colleagues (2001) followed a group of more than 7,500 participants in the longitudinal Health and Retirement Survey (adults ages 51 to 61 at the outset) between 1992 and 1996. The authors compared three groups:1.
those who were continuously insured over the first two years (measured in 1992 and 1994);2.
those who were continuously without insurance over that period; and3.
those who were intermittently uninsured, defined as those who lacked health insurance either in 1992 or in 1994, but not at both times (Baker et al., 2001).
Of those who were continuously uninsured, 22 percent had a major decline17 in self-reported health, 16 percent of the intermittently uninsured experienced a major decline, and 8 percent of the continuously insured reported a major decline in health. In an analysis that controlled for sociodemographic characteristics, preexisting medical conditions, and health behaviors, the authors estimated a 60 percent greater risk of a major decline in health for continuously uninsured persons and a 40 percent greater risk for intermittently insured persons, as compared with continuously insured persons. Continuously or intermittently uninsured persons also had a 20 to 25 percent greater risk of developing a new difficulty in walking or climbing stairs than did those who were continuously insured (Baker et al., 2001).
Cross-Sectional Studies of Health Status
Cross-sectional studies based on large national population surveys (Medical Expenditure Panel Survey [MEPS], National Medical Expenditure Survey [NMES], and Behavioral Risk Factor Surveillance System, provide snapshots of the subjective or self-reported health status of populations according to insurance status. These surveys report worse health status among those without insurance than among those with coverage. Two large studies with careful and extensive analytic adjustments for covarying personal characteristics are presented here.
Franks and colleagues (1993b) examined the relationship between health insurance status and subjective health across several dimensions, including a general health perceptions scale, physical and role functions, and mental health, for 12,000 adults ages 25 through 64. The authors compared participants who had private health insurance for an entire year with those who had been without health insurance the entire year. In an analysis that controlled for age, sex, race, education, presence of a medical condition, and attitude toward medical care and insurance, uninsured adults had significantly lower subjective health scores across all dimensions. The effect on these measures of health of being uninsured was greater for lower-income persons than for those in families with incomes above 200 percent of the federal poverty level, although the effect persisted in both income groups. For both lower- and higher-income adults, the negative effect on perceived health of being uninsured was greater than that of having minority racial or ethnic status. Overall, the extent to which being uninsured negatively affected subjective health (a decrement of 4 points on a 100-point scale) was greater than that of having either of two diseases, cancer or gall bladder disease, and slightly lower than that for arteriosclerosis (Franks et al., 1993b).
Ayanian and colleagues’ (2000) analysis of the 1998 BRFSS compared self-reported health status among adults 18-64 who were uninsured for a year or longer, those uninsured for less than a year, and those with any kind of insurance, public or private. Table 3.1 presents the unadjusted results for the approximately 163,000 adults surveyed. One in five adults uninsured for a year or longer reported being in fair or poor health, compared with one in seven among those uninsured for less than a year, and one in nine for those with health insurance.
TABLE 3.1
Unadjusted Self-Reported Health Status for 18–64 Year-Old Adults, BRFSS, 1998 (percent).
The RAND Health Insurance Experiment
In an experimental study conducted between 1975 and 1982, about 4,000 participants between 14 and 61 years were randomly assigned (in family units) to health insurance plans that differed in the amount of patient cost sharing required, ranging from free care to major deductible plans (95 percent cost sharing, with a maximum of $1,000 per family per year) (Brook et al., 1983; Newhouse et al., 1993). Participants received a lump-sum payment at the beginning of the study to compensate them for their expected out-of-pocket costs if they were in cost-sharing plans. Participants were studied for a three- to five-year period. While persons in plans with any cost sharing had significantly fewer physician visits and hospitalizations than persons in a free-care plan, no difference was found overall between plans with any amount of cost sharing and those with no cost sharing. Free care did result in better outcomes for adults with hypertension, as discussed earlier in this chapter, and in improved visual acuity. This experiment demonstrates both the sensitivity of health care utilization in the general population to cost sharing and the relative insensitivity of short-term (three- to five-year) health outcomes for the general population to cost sharing.
Negative Results
Some studies have reported worse health status for those with health insurance compared to uninsured adults. This result may be attributable to the fact that worse health status may lead to coverage by Medicare or Medicaid, as discussed in Chapter 2 (see Box 2.1) and Chapter 4. However, the competing hypothesis, that health insurance is not associated with overall health status, must also be considered.
Hahn and Flood (1995) used NMES to examine health status by both income level and type and duration of insurance coverage. When SES and demographic characteristics, health behaviors, health care utilization, and Social Security disability status were controlled for in the analysis, self-reported health status was seen to be arrayed from highest to lowest as follows:
- privately insured for the full year,
- privately insured for part of the year and uninsured for part of the year,
- uninsured for the full year,
- publicly insured for part of the year, and
- publicly insured for the full year.
The authors concluded that the likeliest explanation for their results was that the poorer health status of those who qualify for public coverage was not fully accounted for in their analytic model, even though qualification on the basis of disability was considered explicitly (Hahn and Flood, 1995). An alternative (and possibly supplementary) hypothesis was that public insurance—Medicaid specifically—provided enrollees with access and services that were less effective than those provided by private insurance. Neither of these possible explanations can be eliminated based on the research that the Committee has reviewed.
A second study by Ross and Mirowsky (2000) based on the Survey of Aging, Status and the Sense of Control (ASOC) examined the claim that being uninsured contributes to the worse health of persons of lower SES. The ASOC survey included 2,600 adults between ages 18 and 95 at baseline in 1995, 38 percent of whom were 60 years or older. Participants were reinterviewed in 1998 (44 percent were lost to follow-up) (Ross and Mirowsky, 2000). Health status, functional status, and chronic conditions reported by participants at baseline were used to predict health status, functional status, and chronic conditions three years later. Changes in these measures between baseline and follow-up were also included as predictors of health status, functional status, and number of chronic conditions at follow-up in 1998. The authors concluded that privately insured and uninsured persons had similar health status at a three-year follow-up, adjusted for baseline health status, chronic conditions, and sociodemo-graphic characteristics, and that publicly insured persons had worse health status than privately insured and uninsured adults (Ross and Mirowsky, 2000).
The Committee does not find this study convincing in its conclusions because of both the study sample and its analytic design. The sample included a large proportion of persons over 65, all of whom have Medicare, and the substantial fraction of participants lost to follow-up differed systematically from those who were reinterviewed. By including changes in health condition over the study period as independent variables along with health measures at baseline, the authors may have built their findings into the predictive model itself. In addition, Medicare beneficiaries with supplemental health insurance were classified as privately insured; thus, those who counted as publicly insured included only those Medicare beneficiaries without supplemental policies (a lower-income subset of all Medicare beneficiaries) and Medicaid beneficiaries. This atypical classification scheme distorts the comparison between those with public and private health insurance.
CONCLUSION
This chapter has presented studies examining the impact of health insurance status on general measures of population health, on health care and clinical outcomes for specific conditions, and on the appropriate use of preventive services for the nonelderly adult population in the United States. This body of research yields largely consistent and significant findings about the relationship between health insurance and health-related outcomes. In summary, uninsured adults receive health care services that are less adequate and appropriate than those received by patients who have either public or private health insurance, and they have poorer clinical outcomes and poorer overall health than do adults with private health insurance. The specific findings discussed throughout this chapter are presented in Box 3.12.
The Committee has assessed the research regarding the effects of health insurance status across a range of health conditions and services affecting adults. In each domain examined—
- preventive care and screening services,
- cancer care and outcomes,
- chronic disease management and patient outcomes,
- acute care services and outcomes for hospitalized adults, and
- overall health status and mortality,
health insurance improved the likelihood of appropriate care and was associated with better health outcomes. Health insurance appears to achieve these positive effects in part through facilitating ongoing care with a regular health care provider and reducing financial barriers to obtaining those services that constitute or contribute to appropriate care, including screening services, prescription drugs, and specialty mental health services.
Chapter 4 specifically addresses the question of the difference that providing health insurance to uninsured individuals and populations would make to their health and health care. The Committee assesses the potential impact of health insurance coverage on those uninsured adults who are most at risk for poor or adverse health-related outcomes, including the chronically ill, adults in late middle age, members of ethnic minorities, and adults in lower-income households. The chapter also reviews the features and characteristics of health insurance that account for its effectiveness in achieving better health outcomes, including both continuity of coverage and scope of benefits.
NOTES
BOX 4.1Conclusions
The Committee’s conclusions are supported by the evidence and findings presented in Chapter 3, which are largely based on observational studies.
- Health insurance is associated with better health outcomes for adults and with their receipt of appropriate care across a range of preventive, chronic, and acute care services. Adults without health insurance coverage die sooner and experience greater declines in health status over time than do adults with continuous coverage.
- Adults with chronic conditions, and those in late middle age, are the most likely to realize improved health outcomes as a result of gaining health insurance coverage because of their high probability of needing health care services.
- Population groups that are most at risk of lacking stable health insurance coverage and that have worse health status, including racial and ethnic minorities and lower-income adults, particularly would benefit from increased health insurance coverage. Increased coverage would likely reduce some of the racial and ethnic disparities in the utilization of appropriate health care services and might also reduce disparities in morbidity and mortality among ethnic groups.
- When health insurance affords access to providers and includes preventive and screening services, outpatient prescription drugs, and specialty mental health care, it is more likely to facilitate the receipt of appropriate care than when insurance does not have these features.
- Broad-based health insurance strategies across the entire uninsured population would be more likely to produce the benefits of enhanced health and life expectancy than would “rescue” programs aimed only at the seriously ill.
Footnotes
1
Chapter 2 discusses the features of observational (nonexperimental) studies that are necessary for methodological soundness. All quantified study results that are presented in this chapter and in Chapter 4 are significant at least at the 95 percent confidence interval. If results do not meet this level of statistical significance, the confidence interval is reported. See “confidence interval” in Appendix C for further discussion.2
Earlier studies based on the 1986 Access to Care Survey and the 1982 NHIS had findings consistent with those of the more recent nationally representative sample surveys regarding receipt of preventive and screening services by those without health insurance (Hayward et al., 1988; Woolhandler and Himmelstein, 1988).3
Enrollees in private managed care plans is the reference group; however, fee-for-service enrollees did not have significantly different screening rates from those of managed care enrollees. The odds ratio is the relative odds of having an outcome in the uninsured and insured groups. For example, if the odds of receiving a Pap test are 2:1 in a group of uninsured women (i.e., two of every three women or 67 percent receive the test) and the odds are 4:1 in a group of women with insurance (i.e., four of every five women, or 80 percent, receive the test), the odds ratio of uninsured compared to insured women is 0.5 (2:1/4:1). The OR is not a good estimate of the relative risk (the probability of been screened in the uninsured group divided by the probability of being screened in the insured group) because screening is not a rare event. Throughout this report the results of particular studies, if reported as odds ratios or as relative risks, will be presented as the ratio of the uninsured to the insured rates (in this example, as an OR of 0.5).4
Comparing results presented in Potosky et al., 1998, and Breen et al., 2001, the gap in screening rates between insured and uninsured adults decreased between 1992 and 1998.5
Smoking has been associated with an increased risk of colorectal cancer (Chao et al., 2000).6
This hypertension result was an exception to the overall results for the RAND study, which did not find significant differences in outcomes for most conditions and dimensions of health. These results are discussed further in the General Health Outcomes section later in this chapter.7
Notably, this same study found that persons with hypertension who had Medicare coverage only (which does not pay for outpatient prescription drugs) did not have a statistically significant difference in their likelihood of receiving antihypertensive medication than uninsured persons, while those who had Medicare plus Medicaid coverage or Medicare with private supplemental insurance were significantly more likely to have received drug therapy than uninsured persons with hypertension.8
BRFSS has documented the use of recommended services among insured and uninsured persons with diabetes for two recent years. BRFSS collected information on diabetes management in 1994 in 22 jurisdictions (21 states and the District of Columbia) and in 1998 in 37 jurisdictions, representing 70 percent of the U.S. population (Beckles et al., 1998; Ayanian et al., 2000).9
This standard of low hematocrit is below the hematocrit target range of 33–36 percent recommended by the National Kidney Foundation’s Dialysis Outcomes Quality Initiative (NKF, 2001).10
In this study, “late initiation” is defined as glomerular filtration rate of serum creatinine of <5 ml/min per 1.73 m2—a level substantially below both that recommended by the National Kidney Foundation (<10.5 ml/min) and the U.S. mean value at initiation (<7.1 ml/min) (Kausz et al., 2000).11
The HIV Cost and Services Utilization Study (HSCUS), conducted by RAND and the Agency for Healthcare Research and Quality, was a probability sample of persons 18 years and older in the contiguous United States known to have HIV infection who had one visit for regular care (except in a military, prison, or emergency treatment facility) within a two-month period in 1996. Three rounds of interviews were conducted over a two-year period, 1996–1998, with between 2,267 and 2,864 subjects (Shapiro et al., 1999). The AIDS Costs and Utilization Survey, a predecessor study to HCSUS, with six waves over 18 months in 1991 and 1992, was not a probability sample (see Box 2.4 for further detail on these surveys).12
Older studies that examine hospital-based care and outcomes according to insurance status across a range of diagnoses are summarized in Appendix B. The results of these studies are consistent with the findings discussed in text; however, many are based on hospital records that may be less relevant to the current hospital practice environment.13
See Leape et al. (1999) for a description of the RAND methodology for determining appropriateness and its application to developing criteria for revascularization procedures.14
The American College of Surgeons designates hospital EDs as trauma centers based on qualifying criteria related to staffing, resources, and services. There are four designations: Level 1, the most stringent requirements, for providing tertiary care on a regional basis; Level 2, similar services to a Level 1 center but without clinical research and prevention activities; Level 3, presence of emergency services, often in a rural area, with fewer specialized services and resources than Level 1 or 2 centers; and Level 4, usually in a rural area, describing hospitals and clinics that serve a triage function (Bonnie et al., 1999).15
The authors designated an ISS of <16 as “minimal to moderate injury” and >16 as more severe. Overall, 59 percent of transferred patients had an ISS of <9.16
The lowest income category included those with a family income of less than $7,000 at the initial interview (1971–1975).17
A “major decline” in health was defined as a change from excellent, very good, or good health in 1992 to fair or poor health in 1996, or from fair health in 1992 to poor health in 1996 (Baker et al., 2001).